Scroll to:
Three Year Prognosis of Patients with Myocardial Infarction Depending on the Body Weight Index: Data of the Kemerovo Acute Coronary Syndrome Registry
https://doi.org/10.20996/1819-6446-2022-02-08
Abstract
Aim. To study the effect of body mass index (BMI) on the 3-year prognosis of patients after myocardial infarction (MI).
Material and methods. The study is based on data from a 3-year observation of patients with MI from the Kemerovo registry of acute coronary syndrome (n=1366). The characteristics of patients with MI, distributed by the BMI, were determined, the outcomes were analyzed, the risk factors and predictors for the vascular events and mortality were identified.
Results. Obesity was detected in 32.2% people with MI (I degree – 22.3%; II – 7.7%; III – 2.3%), lack of BMI at 0.5%, normal BMI at 20.5%, overweight at 46.9%. Patients with different BMI showed a comparable incidence of recurring MI. In patients with normal BMI, when compared with patients with obesity, unstable angina pectoris (UA), heart failure (HF) and strokes developed often. In patients with normal BMI compared with obese patients, fewer deaths from all causes were recorded within 3 years after MI. A similar pattern with respect to the group with normal BMI in terms of high overall mortality was obtained among patients with overweight who had a lower UA. Patients with obesity was favorable in relation to the development of HF, strokes and overall mortality than patients with overweight. Differences in the 3-year outcomes in the group of patients with MI and underweight were not found when compared with patients with normal and overweight, however, they had a higher of strokes compared with patients with obesity. At patients with I degree obesity within 3 years after MI UA, HF, strokes were less. Patients with III degree obesity, the maximum frequency of total mortality was recorded. The development of death from all causes during the observation period in patients with MI and obesity was associated with: male, smoking, multivessel arterial diseases, non-endovascular reperfusion, acute HF with MI, history of vascular events and angina pectoris; whereas with overweight: multifocal atherosclerosis and arterial hypertension; with a deficit of BMI: non-reperfusion; with normal BMI: heredity for cardiovascular diseases, dyslipidemia and atrial fibrillation.
Conclusion. 3 years after MI patients with obesity of the I degree are less likely than patients with obesity of II-III deaths from all causes are recorded; these patients are less likely than patients with normal weight to develop strokes, HF, UA. Thus, patients with MI and the presence of I degree obesity are characterized by better survival during 3 years of observation.
For citations:
Sedykh D.Yu., German A.I., Hryachkova O.N., Kashtalap V.V., Barbarash O.L. Three Year Prognosis of Patients with Myocardial Infarction Depending on the Body Weight Index: Data of the Kemerovo Acute Coronary Syndrome Registry. Rational Pharmacotherapy in Cardiology. 2022;18(1):4-11. https://doi.org/10.20996/1819-6446-2022-02-08
Introduction
According to the postulates of preventive cardiology, one of the urgent medical and social tasks is the active identification and modification of traditional risk factors for cardiovascular diseases (CVD) [1-3]. One of them is obesity, the frequency of which among the population of developed countries is increasing every year. Today, in the cardiology community, there are conflicting opinions regarding its influence on the formation of early and long-term outcomes in patients with myocardial infarction (MI) despite the active study of this pathological condition [4-7].
To date, society has formed an idea that obesity is associated with a high risk of premature death in the general population, while the maximum number of adverse outcomes, as a rule, falls on the category of people who also have other concomitant conditions: type 2 diabetes mellitus, dyslipidemia, multifocal atherosclerosis, hypertension, atrial fibrillation (AF), chronic obstructive pulmonary disease and chronic kidney disease, osteoporosis and other diseases [8]. At the same time, the role of obesity appears rather as a driver for the further development of more severe diseases, which constitute a prognostically unfavorable metabolic comorbidity. But studies of some registries of patients with coronary heart disease (CHD) [9][10] indicate a possible protective effect of overweight and obesity in the development of acute forms of CHD, which is determined by a decrease in the number of fatal outcomes and recurrent ischemic events in patients with higher than normal indicators, body mass index (BMI) values. Some authors explain this phenomenon by the presence of the so-called «metabolically healthy» and energy-accumulative obesity phenotype, other authors speak of the «obesity paradox», the presence of which and its possible pathophysiological mechanisms are debatable [11-14]. The aim of this study was to study the effect of various BMI indicators on the three-year prognosis in patients after myocardial infarction, given the available conflicting data.
Materials and methods
The study was carried out in accordance with the Declaration of Helsinki of the World Association «Ethical principles for conducting scientific medical research involving humans». The study protocol was approved by the Local Ethics Committee of the Research Institute for Complex Problems of Cardiovascular Diseases. The design of the work is based on a retrospective analysis of the acute coronary syndrome (ACS) registry with ST-segment elevation in Kemerovo with a total number of 1,366 patients included in the registry from 2015 to 2018.
Criteria for inclusion in the study: the presence of a signed informed voluntary consent; the age of patients from 18 to 75 years; diagnosis of ST-segment elevation MI during hospitalization according to current guidelines [15]. Exclusion criteria: low life expectancy of the patient (up to one year) due to the presence of severe concomitant somatic pathology. After the introduction of inclusion/exclusion criteria, the total sample of patients for the study was 875 people. The BMI value was not an inclusion/exclusion criterion, because the data of the initially formed registry were used, which provided for the continuous inclusion of patients with ACS.
At the first stage of the study, all patients with MI were divided into groups depending on the BMI value for further assessment of the obesity prevalence. The obesity group consisted of patients with a BMI ≥30 kg/m2, while BMI values of 30 34.9 kg/m2 corresponded to grade I obesity, 35-39.9 kg/m2 corresponded to grade II obesity, and ≥40 kg/m2 corresponded to grade III obesity. The group with normal body weight consisted of patients with a BMI of 18.5-24.9 kg/m2, with underweight – with a BMI <18.5 kg/m2, with overweight – with a BMI of 25-29.9 kg/m2.
At the second stage of the study, when compared with a group with normal body weight, we assessed the differences in anamnestic risk factors, the clinical course of MI, and treatment tactics in groups of patients with underweight, overweight, and obesity according to BMI. Next, we performed endpoint analysis in all groups within 3 years after MI [death from all causes, recurrent MI, acute cerebrovascular accident (ACV), unstable angina, decompensation of chronic heart failure (CHF)]. We determined predictors of all-cause death in patients within 3 years after MI for each group. Registration of long-term outcomes was carried out using outpatient documentation, discharge epicrises, referrals for post-mortem examination, as well as the results of telephone contacts with patients and/or their relatives.
Statistical processing of the results was performed using the Statistica 10.0 software package (StatSoft Inc., USA). Quantitative indicators are presented as medians (Me) and upper and lower quartiles (25%LQ; 75%UQ), qualitative indicators are presented in absolute numbers (n) and percentages (%). The normality of the distribution was tested using the Kolmogorov-Smirnov's test. Differences in the quantitative indicators of the groups were assessed by the MannWhitney's test. Contingency tables with the subsequent application of Pearson's χ2 test were compiled when assessing qualitative differences. Binary logistic regression with relative risk assessment, bounds of the 95% confidence interval, predictor sensitivity and specificity was used to calculate predictors of death from all causes within 3 years after MI. The critical level of statistical significance was taken as p<0.05.
Results
Obesity was detected in 282 (32.2%) patients. Body weight deficiency was detected in 4 (0.5%) patients, normal body weight was detected in 179 (20.5%), overweight was detected in 410 (46.9%). In the group of patients with obesity according to BMI, patients with grade I obesity amounted to 195 (22.3%) people; II degree – 67 (7.7%); III degree – 20 (2.3%) patients.
Among patients with obesity, compared with patients with normal body weight, there were more women, patients with hypertension, type 2 diabetes, stable angina, but less often there were such factors as smoking, aggravated heredity according to CVD, multifocal atherosclerosis, stroke and myocardial infarction (Table 1). We note when characterizing the hospital stage of the registry study that obese patients were more likely to be referred for coronary angiography followed by stenting, and the incidence of multivessel coronary artery disease was higher. All patients with MI in the hospital were prescribed standard therapy in accordance with clinical recommendations, but patients with obesity for 3 years after MI, compared with patients with normal body weight, were significantly more likely to take beta-blockers, angiotensin-converting enzyme (ACE) inhibitors and statins. Overweight patients differed from patients with normal body weight by a lower incidence of dyslipidemia, smoking and aggravated heredity according to CVD, a history of stroke and myocardial infarction, a higher incidence of hypertension and angina pectoris, and optimal adherence of these patients to antiplatelet, lipid lowering and coronary active therapy for 3 years after MI.
Table 1. Clinical and demographic characteristics of patients with myocardial infarction (n=875)

77 cases of loss of contact with the patient and/or his relatives from the non-obese group were not included in the calculation of endpoints within 3 years after MI, and 69 cases from the obese group. Thus, the final analysis included 213 patients from the obese group, 167 patients from the normal weight group, 4 patients from the underweight group, 345 patients from the overweight group (Table 2). Comparison of patients with different BMI showed a comparable incidence of developing recurrent MI during 3 years of follow-up. Patients with normal body weight, compared with patients with obesity, were more likely to have cases of unstable angina, decompensation of CHF and ACV, but there was a lower incidence of death from all causes within 3 years after myocardial infarction. A similar fact in assessing the incidence of death from all causes was found in overweight patients when compared with patients with normal weight, however, the first patients had fewer cases of unstable angina. At the same time, the group of patients with obesity was more favorable in relation to the lower incidence of CHF, ACV, and mortality from all causes, in contrast to the group of patients with prior MI and overweight. Differences in the outcomes of the patient group with underweight were not obtained in comparison with normal and overweight patients, but a higher frequency of ACV cases was found in them compared with obese patients.
Table 2. Three-year outcomes in patients with myocardial infarction depending on body mass index (n=729)
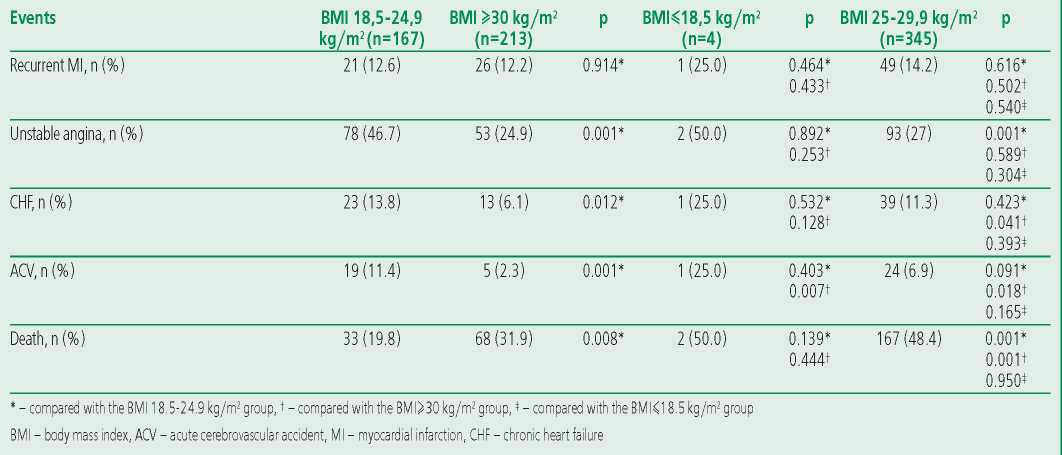
An additional analysis of long-term outcomes of MI showed that patients with grade I obesity were less likely than patients with underweight to have episodes of ACV, less often than patients with overweight, had episodes of ACV, decompensation of CHF, and deaths from all causes, and also less frequently than patients with normal body weight had episodes of unstable angina, CHF and ACV. At the same time, the maximum incidence of death from all causes within 3 years after myocardial infarction was found in patients with myocardial infarction and grade II and III obesity (Table 3).
Table 3. Frequency of outcomes in differentiation of degrees of obesity (n=729)

We used multivariate analysis to determine predictors of overall mortality within 3 years after MI (Table 4). Expected factors associated with overall mortality for patients with MI and obesity were identified: male gender, smoking, multivessel coronary artery disease, failure to perform endovascular reperfusion upon admission to the hospital with MI, course of MI complicated by acute heart failure (AHF), previously suffered vascular events and angina preceding the development of MI.
Table 4. Predictors of three-year mortality in patients with myocardial infarction (n=729)

Thus, the presence of obesity in a male patient with MI is an unfavorable risk factor for the development of a fatal outcome of the disease, compared with female patients. Factors that, regardless of gender differences, worsen the long-term prognosis of a patient after MI were identified as predictors for non-obese patients with MI: multifocal atherosclerosis, hypertension with overweight; failure to perform reperfusion and percutaneous coronary intervention (PCI) upon admission of a patient with MI for patients with underweight; and burdened heredity, dyslipidemia and AF for patients with normal body weight. The development of death from all causes within 3 years was more associated with epidemiological and hereditary risk factors than with adverse metabolic factors in patients with MI without obesity. The presence of grade I obesity in patients with MI was characterized by a certain protective effect on the development of total mortality within 3 years after index MI when compared with patients with grade II and III obesity. At the same time, cases of unstable angina, decompensation of CHF and ACV were more common in patients with myocardial infarction and normal body weight; ACV, CHF decompensation, and deaths from all causes were more common in patients with MI and overweight than in other groups of patients. ACV occurred more often in patients with MI for 3 years with a lack of body weight, compared with other groups.
Discussion
The work proved that the protective, risky or neutral effect of obesity on patients with cardiovascular pathology is pathophysiologically mediated by the complex effect of biological markers of systemic inflammation, the total effect of cardiovascular risk factors and underlying diseases in the anamnesis, as well as the metabolic effects of types of adipose tissue deposition (visceral and subcutaneous) [16].
The present study demonstrates that obesity (grade I in 22.3%, grade II in 7.7%, grade III in 2.3%) was detected among patients with MI in 32.2% of cases. According to our registry study data, obese patients were represented mainly by women with hypertension and type 2 diabetes. According to H.J. Buettner et al. obese patients also had a high prevalence of hypertension (15% higher than in nonobese MI patients), type 2 diabetes (6% higher than in nonobese MI patients) [17]. The Russian register «RECORD-3» and the works of O.A. Kislyak also showed that the majority of patients with MI and obesity were females with clinical characteristics similar to those obtained by us [18][19]. A study of the Spanish database RENACI (Registro Nacional de Comunidades Indígenas, 2007) of patients with various ACS forms, containing data on 824 patients, revealed an association of obesity with risk factors such as angina clinic, prior to the development of MI, and chronic obstructive pulmonary disease in history [20]. A study by M. Kosuge et al found that the presence of obesity was associated with a higher incidence of smoking and cardiac arrhythmias in the early hospital period in 3076 patients with myocardial revascularization performed for MI [21].
According to the results obtained in the present study, patients with MI and obesity were more likely to be referred for coronary angiography followed by PCI with coronary artery stenting, despite a higher number of patients with multivessel coronary atherosclerosis. A similar fact was also in work with the analysis of data from 13,874 coronary angiography performed as part of ACS, where patients had more severe forms of coronary artery disease in the presence of obesity. At the same time, BMI was an independent predictor of the development of non-fatal MI in the long-term follow-up period, along with the absence of revascularization in index MI [20]. The work of M. Zeller et al shows the opposite result, namely, the existing discrimination of patients with MI and obesity in choosing PCI as a reperfusion method, as well as restrictions for such patients in prescribing statins, beta-blockers, and ACE inhibitors in the hospital. At the same time, an increase in BMI per unit was associated with a 5% decrease in 6- and 12-month mortality rates [risk ratio (RR) was 0.95; 95% confidence interval (CI) ranged from 0.93 to 0.98; p<0.001] [22]. Research by M.H. Seo and W.Y. Lee made it possible to establish that PCI in patients with MI and obesity didn't significantly optimize the prognosis of this patient category [23], in contrast to patients with MI without obesity.
The present study demonstrated a favorable threeyear outcome among patients with MI with obesity, compared with patients with normal body weight, who more often developed cases of unstable angina, ACV, and decompensated CHF. This result is consistent with the data of the Korean registry of ACS with ST segment elevation in KAMIR (Korea Acute Myocardial Infarction Registry score, 2011), where a favorable prognosis was more often observed in patients with obesity compared with patients with underweight [24]. Attempts to systematize 40 studies with 250,152 patients over 3.8 years, undertaken by A. Romero-Corral et al, found that patients with obesity (BMI=30- 35kg/m2) had a risk of general [RR=0.93, 95% CI=0.85-1.03)] and cardiovascular mortality [RR=0.97, 95% CI=0.82-1.15)] was lower compared to those for patients with lower BMI values [25]. We note that in the era of «pre-reperfusion studies», mortality within 12 months after MI in patients with obesity and normal body weight didn't differ, and after a year of follow-up it was lower in the obese group. In the studies of L. Mehta and D.B. Diercks et al., optimal survival after invasive myocardial revascularization was also shown in patients with elevated BMI, regardless of the initial type of MI [26][27]. In contrast, the MERLIN-TIMI 36 protocol (Metabolic Efficiency with Ranolazine for Less Ischemia in NonST Elevation Acute Coronary Syndromes, 2006) in patients with ACS didn't associate hospital endpoints with high BMI, while showing evidence of high heart vascular death rate and recurrent MI in patients with normal and low BMI values [28]. A study by C. Lazzeri et al also revealed a protective effect of obesity on the development of endpoints only in grade I, but in patients under 75 years of age [29]. At the same time, many authors attribute the protective mechanism of obesity to the fact that an increase in BMI values increases the diameter of the coronary arteries and improves myocardial perfusion and its volumetric blood flow [34-36]. Rea T.D. et al showed that the risk of recurrent MI during the first year of follow-up increases with the severity of obesity in post-MI patients [30]. At the same time, a large non-randomized meta-analysis, including 36 studies, showed that direct revascularization of the infarctdependent artery didn't reduce the risk of long-term death in patients with ACS at high BMI values [23][25].
The development of deaths within 3 years among obese patients after MI in this study was mainly associated with a history of angina, smoking, MI and stroke, as well as with male gender, multivessel coronary artery disease, failure to perform a stenting procedure and complicated course of MI in the form of AHF. AHF as a complication of MI influenced the frequency of long-term adverse outcomes in the group of patients with ACS without obesity according to the study by W.Y. Kang et al., where they also found lower serum concentrations of NT-proBNP in overweight patients [31]. The association of known risk factors (male gender, smoking, and multivessel coronary artery disease) was also identified with the development of adverse endpoints in the long-term period after MI in the Gulf RACE-2 registry (Gulf Registry of Acute Coronary Events, 2012) [32] and in works of G.A. Chumakova [12][33]. The work of Barnaul colleagues also revealed a relationship between the visceral type of obesity and adverse long-term outcomes of MI.
According to N.M. Morris et al., the risk of allcause mortality predominated in severely obese patients with low left ventricular ejection fraction in the absence of restoration of coronary perfusion and insufficient effect of conservative therapy [34]. In the present study, we found that the predictors of overall mortality in patients without obesity were multifocal atherosclerosis, aggravated heredity in CVD, AF, dyslipidemia, hypertension, and failure to perform pharmacological reperfusion in MI without the possibility of PCI. The latter is due to the fact that non-obese MI patients more often came from remote regions of the Kemerovo region, where thrombolytic therapy is the optimal method of reperfusion.
Thus, the significance of diagnosing changes in body weight (both underweight and overweight with obesity) according to BMI in assessing the longterm prognosis of MI is beyond doubt.
This study demonstrates that there is a certain «protective» effect in relation to a lower incidence of death from all causes in patients with myocardial infarction within 3 years when grade I obesity is established, in contrast to the absence of such an effect when obesity II and III are established. Apparently, the lack of unity of views on the prognostic role of obesity in MI is due to this. We need to continue studying the clinical and prognostic significance of obesity in myocardial infarction using other detection criteria, including data from radiation methods of assessment, as well as to determine the possible pathogenetic mechanisms of the protective effect of mild obesity on patient survival in the postinfarction period.
Study limitation: single-center nature of the registry; the use of BMI as a method for assessing obesity, which doesn't determine the division into visceral and subcutaneous components.
Conclusion
Deaths from all causes within 3 years after myocardial infarction are recorded less frequently in patients with grade I obesity than in patients with grade II-III obesity; these patients also were less likely than patients with normal body weight to have vascular events: cerebral strokes, decompensated heart failure, unstable angina. Thus, patients with prior myocardial infarction and grade I obesity are characterized by better survival during 3 years of follow-up, compared with other groups of patients distributed by BMI.
Relationships and Activities. None.
Funding: The study was performed with the support of the Research Institute for Complex Issues of Cardiovascular Diseases. The research was made within the fundamental research project of the Research Institute for Complex Issues of Cardiovascular Diseases «Multivessel coronary artery disease, polyvascular disease and comorbid conditions. The diagnosis and risk management in a large industrial region of Siberia».
References
1. Lavie CJ, Milani RV, Ventura HO, et al. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53(21):1925-32. DOI:10.1016/j.jacc.2008.12.068.
2. Angelantonion ED, Bhupathiraju SN. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-86. DOI:10.1016/S0140-6736(16)30175-1.
3. Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211-9. DOI:10.1056/NEJMoa1000367.
4. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766-81. DOI:10.1016/s0140-6736(14)60460-8.
5. Lavie J, McAuley PA, Church TS, et al. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol. 2014;63(14):1345-54. DOI:10.1016/j.jacc.2014.01.022.
6. Niedziela J, Hudzik B, Niedziela N, et al. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur J Epidemiol. 2014;29(11):801-12. DOI:10.1007/s10654-014-9961-9.
7. Lamelas P, Schwalm JD, Quazi I, et al. Effect of body mass index on clinical events after acute coronary syndromes. Am J Cardiol. 2017;120(9):1453-9. DOI:10.1016/j.amjcard.2017.07.043.
8. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(2):342-62. DOI:10.1210/jc.2014-3415.
9. Bucholz EM, Rathore SS, Reid KJ, et al. Body mass index and mortality in acute myocardial infarction patients. Am J Med. 2012;125(8):796-803. DOI:10.1016/j.amjmed.2012.01.018.
10. Wienbergen H, Gitt A, Juenger C. Impact of the body mass index on occurrence and outcome of acute ST-elevation myocardial infarction. Clin Res Cardiol. 2008;97(2):83-8. DOI:10.1007/s00392-007-0585-x.
11. Romantsova TI, Ostrovskaya EV. Metabolically healthy obesity: definitions, protective factors, clinical relevance. Almanac of Clinical Medicine. 2015;1(1):75-86 (In Russ.) DOI:10.18786/2072-0505-2015-1-75-86.
12. Ott AV, Chumakova GA. Epicardial obesity as one of the basic criteria for metabolically unhealthy obesity phenotype and the predictor of subclinical atherosclerosis. Complex Issues of Cardiovascular Diseases. 2018;7(1):21-8 (In Russ.) DOI:10.17802/2306-1278-2018-7-1-21-28.
13. Kapoor JR, Heidenreich PA. Obesity and survival in patients with heart failure and preserved systolic function: a U-shaped relationship. Am Heart J. 2010;159(1):75-80. DOI:10.1016/j.ahj.2009.10.026.
14. Fonarow GC, Srikanthan P, Costanzo MR, et al. An obesity paradox in acute heart failure: analysis of body mass index and in-hospital mortality for 108,927 patients in the Acute Decompensated Heart Failure National Registry. Am Heart J. 2007;153(1):74-81. DOI:10.1016/j.ahj.2006.09.007.
15. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-77. DOI:10.1093/eurheartj/ehx393.
16. Garvey WT, Garber AJ, Mechanick JI, et al.; The Aace Obesity Scientific Committee. American association of clinical endocrinologists and american college of endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pract. 2014;20(9):977-89. DOI:10.4158/EP14280.PS.
17. Buettner HJ, Mueller C, Gick M, et al. The impact of obesity on mortality in UA/non-ST-segment elevation myocardial infarction. Eur Heart J. 2007;28(14):1694-701. DOI:10.1093/eurheartj/ehm220.
18. Erlikh AD. Twelve months outcomes in patients with acute coronary syndrome, by the national registry RECORD-3. Russian Journal of Cardiology. 2018;(3):23-30 (In Russ.) DOI:10.15829/1560-4071-2018-3-23-30.
19. Kislyak OA, Starodubova AV, Khautieva FM, et al. Myocardial infarction in women with overweight and obesity. Consilium Medicum. 2010;(10):26-31. (In Russ.)
20. Kosuge M, Kimura K, Kojima S, et al. Impact of body mass index on in-hospital outcomes after percutaneous coronary intervention for ST segment elevation acute myocardial infarction. Circ J. 2008;72(4):521-5. DOI:10.1253/circj.72.521.
21. Zeller MH, Inge TH, Modi AC, et al. Severe obesity and comorbid condition impact on the weight-related quality of life of the adolescent patient. J Pediatr. 2015;166(3):651-9.e4. DOI:10.1016/j.jpeds.2014.11.022.
22. Seo MH, Lee WY, Kim SS, et al. Committee of Clinical Practice Guidelines, Korean Society for the Study of Obesity (KSSO). J Obes Metab Syndr. 2019;28(1):40-5. DOI:10.7570/jomes.2019.28.1.40.
23. Kim HK, Jeong MH, Ahn Y, et al. Hospital discharge risk score system for the assessment of clinical outcomes in patients with acute myocardial infarction (Korea Acute Myocardial Infarction Registry [KAMIR] score). Am J Cardiol. 2011;107(7):965-71. DOI:10.1016/j.amjcard.2010.11.018.
24. Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666-78. DOI:10.1016/S0140-6736(06)69251-9.
25. Mehta L, Delvlin W, McCullough PA, et al. Impact of body mass index on outcomes after percutaneous coronary intervention in patients with acute myocardial infarction. Am J Cardiol. 2007;99(7):906-10. DOI:10.1016/j.amjcard.2006.11.038.
26. Diercks DB, Roe MT, Mulgund J, et al. The obesity paradox in non-ST-segment elevation acute coronary syndromes: results from the Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the American College of Cardiology/American Heart Association Guidelines Quality Improvement Initiative. Am Heart J. 2006;152(1):140-8. DOI:10.1016/j.ahj.2005.09.024.
27. Morrow DA, Scirica BM, Karwatowska-Prokopczuk E, et al. Effects of ranolazine on recurrent cardiovascular events in patients with non-ST-elevation acute coronary syndromes: the MERLIN-TIMI 36 randomized trial JAMA. 2007;297(16):1775-83. DOI:10.1001/jama.297.16.1775.
28. Lazzeri G, Pammolli A, Pilato V, et al. Relationship between 8/9-yr-old school children BMI, parent’s BMI and educational level: a cross sectional survey. Nutr J. 2011;10(76):1-8. DOI:10.1186/1475-2891-10-76.
29. Norris RM, Caughey DE, Mercer CJ, et al. Prognosis after myocardial infarction. Six-year follow-up. Br Heart J. 1974;36(8):786-90. DOI:10.1136/hrt.36.8.786.
30. Rea TD, Heckbert SR, Kaplan RC, et al. Body mass index and the risk of recurrent coronary events following acute myocardial infarction. Am J Cardiol. 2001;88(5):467-72. DOI:10.1016/s0002-9149(01)01720-9.
31. Kang WY, Jeong MH, Ahn YK, et al. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol. 2010;55(1):84-91. DOI:10.1016/j.jjcc.2009.10.004.
32. Alhabib KF, Sulaiman K, Al-Motarreb A, et al. Baseline characteristics, management practices, and long-term outcomes of Middle Eastern patients in the Second Gulf Registry of Acute Coronary Events (Gulf RACE-2). Ann Saudi Med. 2012;32(1):9-18. DOI:10.5144/0256-4947.2012.9.
33. Chumakova GA, Kuznetsova TY, Druzhilov MA, et al. Visceral adiposity as a global factor of cardiovascular risk. Russian Journal of Cardiology. 2018;(5):7-14 (In Russ.) DOI:10.15829/1560-4071-2018-5-7-14.
About the Authors
D. Yu. SedykhRussian Federation
Darya Yu. Sedykh.
Kemerovo.
A. I. German
Russian Federation
Albina I. German.
Kemerovo.
O. N. Hryachkova
Russian Federation
Oksana N. Khryachkova.
Kemerovo.
V. V. Kashtalap
Russian Federation
Vasily V. Kashtalap.
Kemerovo.
O. L. Barbarash
Russian Federation
Olga L. Barbarash.
Kemerovo.
Review
For citations:
Sedykh D.Yu., German A.I., Hryachkova O.N., Kashtalap V.V., Barbarash O.L. Three Year Prognosis of Patients with Myocardial Infarction Depending on the Body Weight Index: Data of the Kemerovo Acute Coronary Syndrome Registry. Rational Pharmacotherapy in Cardiology. 2022;18(1):4-11. https://doi.org/10.20996/1819-6446-2022-02-08














































