Rational Pharmacotherapy in Cardiology is a peer-reviewed scientific and practical journal for cardiologists and therapists, published since 2005 with the support of the Russian Society of Cardiology and the National Medical Research Center for Therapy and Preventive Medicine. The Editor-in-Chief is Oksana M. Drapkina, MD, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Sciences.
Rational Pharmacotherapy in Cardiology is a nationwide Russian journal published 6 times a year.
Its content includes original scientific articles, national guidelines, scientific reviews, lectures, and the results of clinical practice analysis. The journal covers issues of early diagnosis, primary and secondary prevention of cardiovascular diseases and comorbid conditions, effective pharmacotherapy, and current topics in experimental and clinical pharmacology.
The journal is indexed in
- The List of Publications of the Higher Attestation Commission (HAC, K1)
- The Russian Science Citation Index (RSCI)
- Web of Science and Scopus international databases
Open Access Journal (OA, DOAJ).
Full-text issues are available on the Scientific Electronic Library website (www.elibrary.ru) and the journal’s website (https://www.rpcardio.online/jour).
For Authors: Submission guidelines: https://www.rpcardio.online/jour/about/submissions#authorGuidelines
Subscription: http://roscardio.ru/ru/subscription.html
ISSN 1819-6446 (Print)
ISSN 2225-3653 (Online)
The journal was registered on 30.12.2004 and re-registered by Roskomnadzor on 31.03.2022 (PI no. FS 77-82859)
Founder — FSBI "National Medical Research Center for Therapy and Preventive Medicine" of the Ministry of Health of the Russian Federation
Circulation: 5000. Frequency: 6 issues a year
Higher Attestation Commission: 140105 Cardiology, 140306 Pharmacology, Clinical Pharmacology.
3.1.20. Cardiology (Medical Sciences), 3.3.6. Pharmacology, Clinical Pharmacology (Medical Sciences) since 01.02.2022 3.1.18. Internal Medicine (Medical Sciences), 3.1.31. Gerontology and Geriatrics (Medical Sciences) since 08.07.2024
Metrics:
- Two-year RSCI impact factor (2023): 1.019
- SCIENCE INDEX ranking: 9
- Ranked 22nd in the "Medicine and Healthcare" category
Current issue
ORIGINAL STUDIES
Aim. To assess adherence to pharmacotherapy and access to state-sponsored drug coverage (SSDC), as well as to identify factors influencing treatment adherence within a year after myocardial infarction (MI).
Material and methods. This observational multicentre study included a sample of patients with MI hospitalized in 13 regions of the Russian Federation from June 2015 to August 2016. The study included 1107 patients with MI aged 35-75 years. Using the Morisky-Green compliance scale (MMAS-4), an analysis of treatment adherence was performed in 889 patients 12 months after MI. Anamnestic data were also collected, a survey was conducted on the receipt of SSDC to identify factors associated with high treatment adherence.
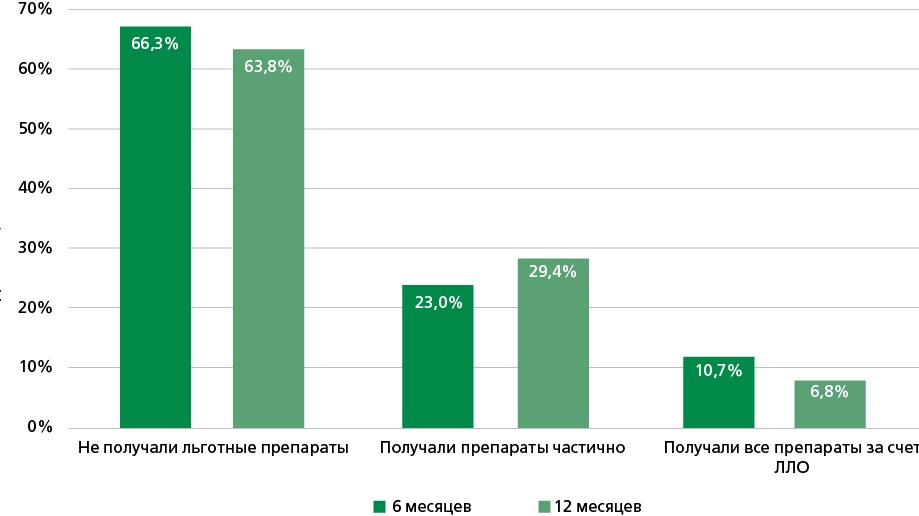
Results. At 12 months after MI, 59.9% of patients were fully adherent to treatment, 21.8% were insufficiently adherent, and 18.3% were not adherent to drug therapy. Men were less adherent to treatment than women (p=0.003), and younger patients were less adherent than older patients (p=0.028). 10.7% of patients received medications at the expense of the SSDC after 6 months, and 6.5% of patients after 12 months. Older age group individuals (p<0.001) and women (p=0.006) received subsidized medications significantly more often. The factors associated with receiving SSDC were contacts with the healthcare system: observation by a therapist (OR 1.53; CI: 1.01-2.34; p=0.044), cardiologist (OR 1.61; CI: 1.04-2.51; p=0.035), dispensary observation (OR 3.56; CI: 2.2-6.22; p<0.001), rehospitalization (OR 1.57; CI: 1.03-2.39; p=0.036). The only factor significantly associated with a reduced likelihood of receiving SSDC was smoking (OR 0.54; CI: 0.33-0.9; p=0.018).
Conclusion. The results of this study revealed insufficient patient treatment adherence during the year after MI. Men and young patients were less adherent to treatment. We observe a small percentage of full subsidized drug provision (6.5%), however, at the time of the study, patients with MI without disabilities and social benefits did not qualify for subsidized provision programs. Patients who had contact with the healthcare system were significantly more likely to receive preferential SSDC: those who had been to a cardiologist or therapist, were under dispensary observation, were re-hospitalized. The only factor significantly associated with a decrease in the likelihood of receiving preferential drug provision was smoking. Among the factors reliably associated with high adherence to treatment according to the results of this study, one can highlight the presence of a stroke in the anamnesis. Receipt of preferential drug provision during the year after MI did not reliably affect adherence.
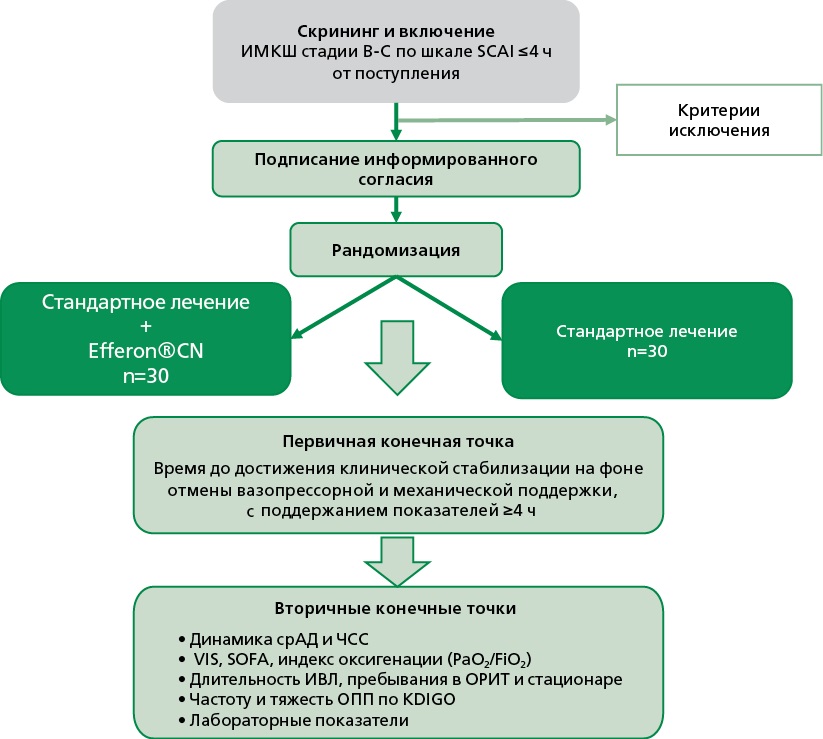
Aim. To evaluate the efficacy and safety of cytokine hemoadsorption using the Efferon®CT device in patients with myocardial Infarction-associated shock at SCAI (Society for Cardiovascular Angiography and Interventions) stages B-C.
Material and methods. This is a protocol of an open-label, single-center, randomized controlled clinical trial. A total of 60 patients aged 18-80 years with myocardial Infarction-associated shock diagnosed within 4 hours prior to randomization will be enrolled. Participants will be randomized (1:1) to the intervention group (standard therapy + hemoadsorption, n=30) or the control group (standard therapy, n=30). Primary endpoint: time to clinical stabilization (hemodynamic normalization with discontinuation of vasopressor and mechanical support, sustained ≥4 hours). Secondary endpoints: hemodynamic parameters, oxygenation index, SOFA (Sequential Organ Failure Assessment) score, incidence of acute kidney injury (Kidney Disease: Improving Global Outcomes, KDIGO), duration and need for mechanical ventilation, intensive care unit and hospital length of stay, dynamics of inflammatory and organ function markers.
Expected results. Hemoadsorption with Efferon®CT is expected to remove pro-inflammatory molecules of medium molecular weight, thereby improving macro- and microcirculation, reducing multiple organ dysfunction, and decreasing the need for vasopressor support.
Conclusion. This study aims to provide the first evidence on the efficacy and safety of early cytokine hemoadsorption in myocardial Infarction-associated shock. The findings may support its pathophysiological rationale and form the basis for large-scale multicenter trials and potential updates of clinical practice guidelines.
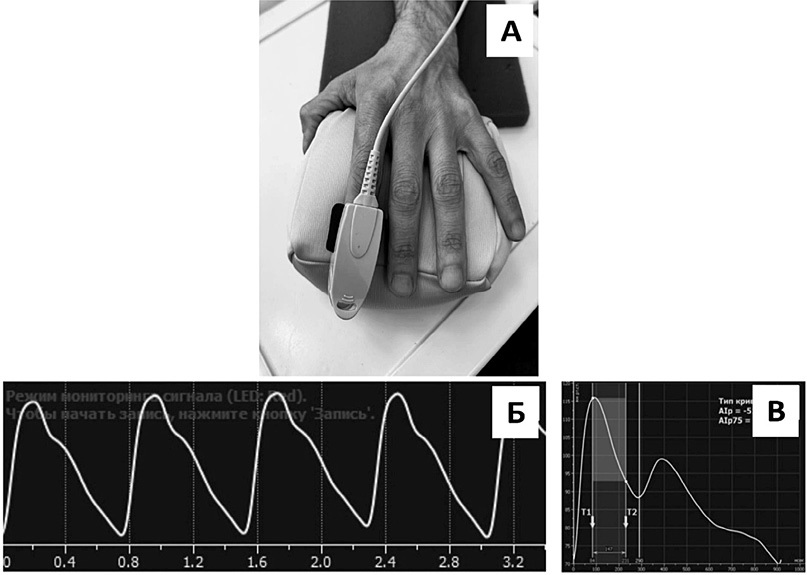
Aim. To study the functional state of terminal muscular arteries and distributing arterioles using transmission photoplethysmography (PPG) in men of working age with different levels of psychosocial stress (PS).
Material and methods. 200 men (50.9±1.0 years) underwent physical examination, anthropometry, assessment of the PS level using the Reeder test adapted by O. S. Kopina, biochemical blood test (total cholesterol (TC) and lipid profile, glucose, C-reactive protein), 24-hour ambulatory blood pressure monitoring (ABPM) and transmission PPG of the left-hand index finger. All subjects were classified into 5 ordered groups depending on the distribution of stress indicators by quintiles: Group 1 consisted of 43 men with low stress level (3.57-4.0 points), Group 2 – 38 men with medium-low level (3.28-3.43 points), Group 3 – 41 men with medium level (2.9-3.14 points), Group 4 – 47 men with medium-high level (2.57-2.9 points), and Group 5 – 31 men with high stress level (1.43-2.57 points).
Results. The results of the primary analysis demonstrated a significant increase in pulse wave velocity (aSI) in working-age men with increasing PS level (p=0.042), as well as a non-significant trend towards greater vascular stiffness (Alp75) of terminal muscular arteries and distributing arterioles in the moderate and moderatehigh PS groups (p=0.089). Results of multiple regression analysis adjusted for body mass index, ABPM, smoking, cholesterol, and drug therapy demonstrated that arterial stiffness (Alp75) was higher in the groups with medium (B=6.18; p=0.026) and medium-high (B=6.27; p=0.023) PS levels compared to high. No reliable associations were found between the PS level and the pulse wave velocity (aSI) and smooth muscle tone (RI) of the studied vessels in men of working age.
Conclusion. In men of working age with medium and medium-high PS levels, an increase in vascular stiffness, in addition to elastic and large-elastic arteries, can also develop at the level of terminal muscular arteries and distributing arterioles. Reducing the level of PS with a possible concomitant decrease in arterial stiffness in order to reduce the risk of development and progression of cardiovascular diseases and improve the quality of life of patients seems to be an urgent therapeutic task.
Aim. To study the associations of N-terminal pro-brain natriuretic peptide (NT-proBNP) level with body composition parameters in comparison with body mass index (BMI) in men with chronic heart failure (CHF).
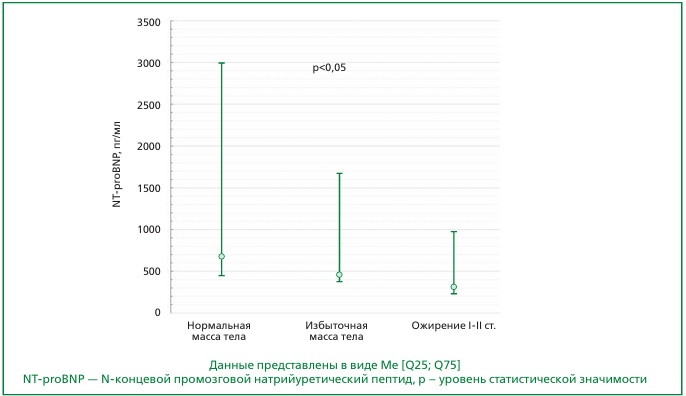
Material and methods. The study included 60 men aged 20-70 years with CHF of various etiologies and reduced or mildly reduced left ventricular ejection fraction (LVEF). The BMI was calculated using the Quetelet formula: [BMI = body weight (kg)/height (m2)]. Quantitative body composition (fat, muscle, and bone mass) was determined using dual-energy X-ray absorptiometry. NT-proBNP level was determined with method of chemiluminescent enzyme immunoassay using MAGTRATION technology.
Results. NT-proBNP level in men with normal body weight was significantly higher than in overweight and obese individuals (680 [427; 2994], 446 [381; 1667], 300 [226; 967] pg/ml (p<0.05), respectively). The amount of both fat and muscle mass was significantly higher in obese individuals, however, in a linear regression analysis adjusted for age NT-proBNP levels were independently associated only with the appendicular muscle mass and the appendicular skeletal muscle index.
Conclusion. Patients with CHF and obesity have lower NT-proBNP values than those with normal body weight. An independent inverse association of NT-proBNP level with BMI and with indicators of muscle mass, but not body fat, was demonstrated. These findings suggest that the muscle component of body weight contributes to the lower NT-proBNP values in CHF patients with high BMI.
Aim. To evaluate the impact of early administration of empagliflozin — from the first day of treatment of acute decompensated heart failure (ADHF) on outcomes at 3 and 6 months.
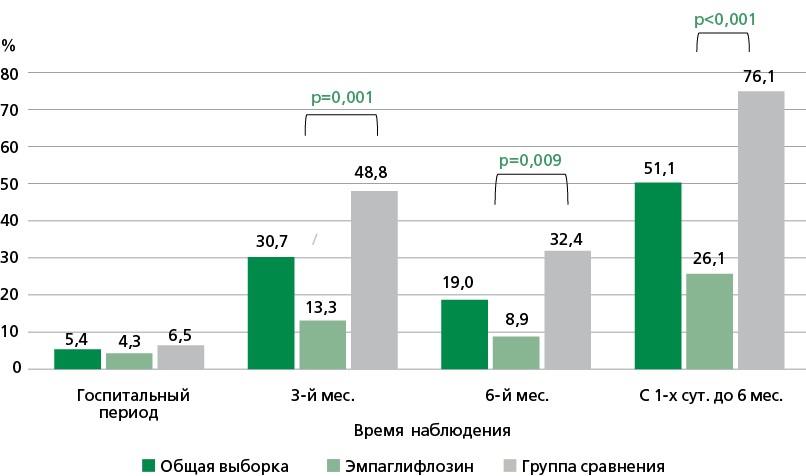
Material and methods. The study included 92 patients admitted to the hospital with ADHF without hemodynamic instability. On the 1st day of hospitalisation, patients were included in the study and were randomized to receive empagliflozin at a daily dose of 10 and 25 mg (in case of ineffective glycemic control for patients with type 2 diabetes mellitus) into two equal groups. The patients in the comparison group received treatment without gliflozines during the hospital period of the study, however, upon discharge from the hospital, empagliflozin or dapagliflozin was recommended along with other prescriptions, while 8 patients started taking this class of drug.: 7 — within 3 months after discharge from the hospital, 1 — during the 3rd — 6th month of the study. Data on the development of adverse cardiovascular events and surgical interventions for cardiovascular diseases, as well as side effects and adverse events associated with empagliflozin therapy were collected from all participants at each stage of inpatient and outpatient follow-up (3 and 6 months after discharge from the hospital).
Results. Of the 92 study participants, there were 18 (19,6%) deaths (all due to ADHF) and 9 (9,8%) nonfatal cardiovascular events over the 6-month period. Over the entire observation period, a lower number of all cases of adverse cardiovascular events were observed in the empagliflozin group (26,1% vs 76,1%, p <0,001). Kaplan-Meier analysis showed significant differences in survival, as well as in the time to any adverse event (death or nonfatal event), depending on the use of empagliflozin within 6 months after the ADHF episode: 6,5% vs 32,6% (p=0,002) and 15,2% vs 43,5% (p=0,003), respectively. When analyzing the outcomes in individual study periods (day of discharge — month 3; months 3 — 6), the frequency of adverse events was significantly lower in the main group (13,3% vs 48,8%, p=0,001; 8,9% vs 32,4%, p=0,009, respectively), and a difference was noted in the frequency of fatal outcomes at month 3 (0% vs 20,9%) and non-fatal events at month 6 (0% vs 14,7%) depending on the intake of empagliflozin. No adverse reactions or undesirable effects were registered during therapy.
Conclusion. Treatment of patients with ADHF with empagliflozin at a dose of 10 mg/day from the first day of hospitalisation is safe and improves the prognosis (mortality and recurrent ADHF episodes) at 3 and 6 months after hospital discharge.
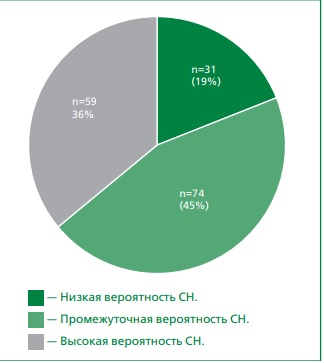
Aim. To assess the prognostic value of left atrial reservoir strain for predicting the risk of major adverse cardiovascular events in patients with type 2 diabetes (T2D) and intermediate probability of heart failure with preserved ejection fraction (HFpEF) over a 1-year follow-up period.
Material and methods. A prospective study initially screened 164 patients with T2D (mean age 61±8 years) presenting with dyspnea and preserved left ventricular ejection fraction (≥50%). Using the HFA-PEFF score: HFpEF was considered unlikely with ≤1 point and confirmed with ≥5 points. The final study cohort comprised 58 patients with intermediate HF probability (2-4 points). These patients underwent standard clinical assessment, including laboratory and instrumental tests, as well as diastolic stress echocardiography (DSE) with physical exercise on a horizontal bicycle ergometer. A positive DSE result was defined as either: 1) an increase in E/e’ ratio ≥15 during exercise (2 points), or 2) an increase in E/e’≥15 accompanied by tricuspid regurgitation velocity >3.4 m/s (3 points). Left atrial strain (LAS) was assessed using speckle-tracking echocardiography with focus on reservoir function, with abnormal values defined as ≤18%.
Results. According to DSE, 29.3% of patients had a positive result, confirming a diagnosis of heart failure with preserved ejection fraction (HFpEF). This group exhibited significantly lower LAS values both at rest and during exercise. Reduced LAS during exercise was correlated with increased left ventricular filling pressure. Furthermore, LAS demonstrated independent prognostic value in assessing the risk of adverse events. Kaplan-Meier analysis revealed a statistically significant association between LAS ≤18% and the risk of reaching the composite endpoint in the HFpEF group (Log Rank = 14.72; p <0,001).
Conclusion. In patients with type 2 diabetes and intermediate HFpEF probability, reduced left atrial reservoir strain (≤18%) is a significant predictor of adverse cardiovascular events within a 1-year follow-up period.
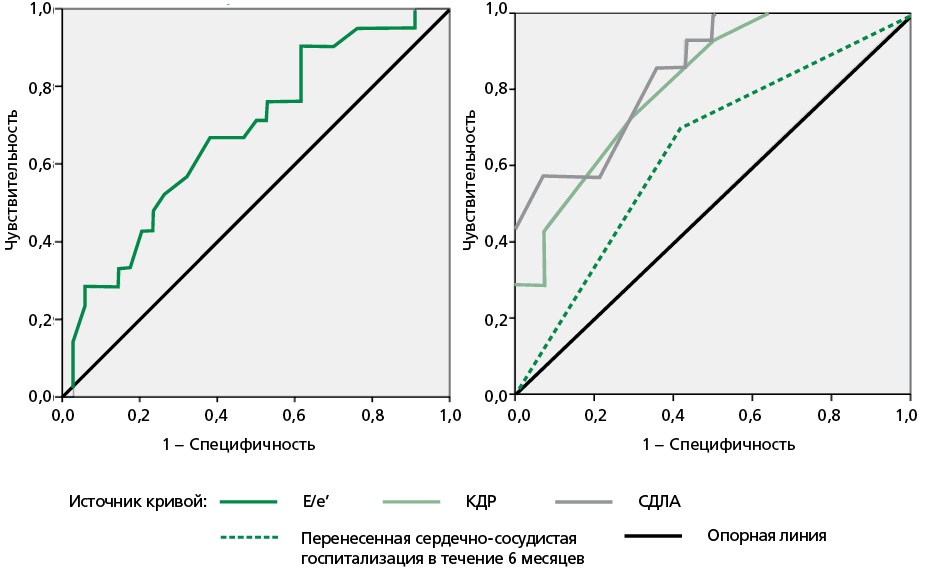
Aim. To study the biomarker profile, clinical and echocardiographic characteristics of patients with the “cardio-reno-metabolic phenotype” of heart failure with preserved ejection fraction (HFpEF), as well as their impact on the six-month prognosis.
Material and methods. A prospective study of 80 patients with “cardio-reno-metabolic phenotype” of HFpEF was conducted. Anamnesis, clinical and demographic data, concomitant pathology were analyzed, enzyme immunoassay of blood serum was performed to determine the concentrations of the N-terminal fragment of brain natriuretic peptide (NT-proBNP), galectin-3, soluble form of tumor suppressor 2 (sST2), hypoxia-inducible factor 1-alpha (HIF-1α), carboxymethyllysine (CML), a six-minute walk test and echocardiographic examination with assessment of left ventricular diastolic function were performed.
Results. On average, the NT-proBNP level was 125.8 [109.4; 146.9] pg/ml, galectin-3 — 1.2 [0.9; 1.4] ng/ml, sST2 — 1.5 [0.4; 3.8] ng/ml, HIF-1α — 0.13±0.049 ng/ml, CML — 346.69±50.63 pg/ml. Within six months, 36.3% of patients were rehospitalized for any reason, 18.8% of them for cardiovascular diseases. A history of hospitalisation for a cardiovascular cause (decompensated CHF, uncontrolled hypertension, angina, rhythm disturbance) was an important risk factor for rehospitalisation during the six-month observation period. Using ROC analysis and binary logistic regression, clinical, laboratory, and instrumental predictors of early rehospitalisation for cardiovascular causes were identified: a history of such hospitalisation within the previous 6 months, left ventricular enddiastolic dimension greater than 5.05 cm, systolic pulmonary artery pressure greater than 24.5 mm Hg, H2FPEF score greater than 6.5 points, glomerular filtration rate less than 36.97 ml/min/1.73m², Charlson Comorbidity Index greater than 5.5 points, and galectin-3 level less than 1.5 ng/ml . Based on the data obtained, a model for predicting re-hospitalisation during 6 months of observation was developed, the sensitivity of which was 66.7%, specificity — 89.1%.
Conclusion. Predictors of early rehospitalisation for cardiovascular reasons for patients with the “cardio-reno-metabolic phenotype” of HFpEF include the history of hospitalisation for cardiovascular reasons in the previous 6 months, an increase in the left ventricular end-diastolic dimension, elevated systolic pulmonary artery pressure, decreasedglomerular filtration rate, Charlson comorbidity index, galectin-3 level, and the mean H2FPEF score.
Aim. To evaluate the risk factors for the development of cardiac conduction disorders and to determine their significance in temporary and permanent pacemaker implantation in patients after surgical aortic valve replacement and other combined cardiac surgical interventions.
Material and methods. The analysis of patients who underwent surgical aortic valve replacement and other combined cardiac surgical interventions for the period from January 2018 to May 2023 in Krasnoyarsk Regional Clinical Hospital was performed.
Results. The correlation between the occurrence of atrioventricular block (AVB) of II-III degree and sinus node dysfunction (SND) that required temporary pacemaker and permanent pacemaker implantation in patients after surgical prosthesis of aortic valve and other combined cardiac surgical interventions was determined. After AVR and other combined cardiac interventions atrial fibrillation (AF) was detected in 107 (44.6%) patients, left bundle branch block (LBBB) and right bundle branch block (RBBB) in 8 (3.3%) patients, and first-degree AV block in 12 (5.0%) patients. The need for temporary pacemaker after surgical prosthetic aortic valve and other combined cardiac surgical interventions was in 79 (45.4%) patients. 76 (96.2%) patients underwent TCP within 2 days after surgical treatment and 3 (3.8%) patients within 72 hours. According to single-factor analysis, 4 important reasons for required temporary pacemaker were identified: atrial fibrillation (OR=2,47, 95% CI=1,31-4,46, p=0,005), age older than 58.5 years (OR=2,52, 95% CI=1,29-4,93, p=0,006), glomerular filtration rate less than 77 ml/min (OR=2,12, 95% CI =1,08-4,17, p=0,028) and atrial tachycardia (OR=8,00, 95% CI=1,04-67,92, p=0,046). Рermanent pacemaker implantation was performed in 12 (6.7%) patients, 11 (91.7%) due to complete AVB and 1 (8.3%) patient due to SVD development. Pacemaker implantation after cardiac surgery was performed in 8 (66.7%) patients from 5 to 8 days, 3 (25.0%) patients from 10 to 15 days, and 1 (8.3%) patient after 23 months. According to regression analysis, a significant sign indicating a high risk of pacemaker implantation — presence of baseline left bundle branch block (OR= 6,32, 95% CI=1,09-36,70, p=0.020).
Conclusion. The identified risk factors for conduction disturbances after aortic valve replacement and other cardiac surgical interventions can be used for timely conduction and implantation of a permanent pacemaker.
PAGES OF RUSSIAN NATIONAL SOCIETY OF EVIDENCE-BASED PHARMACOTHERAPY
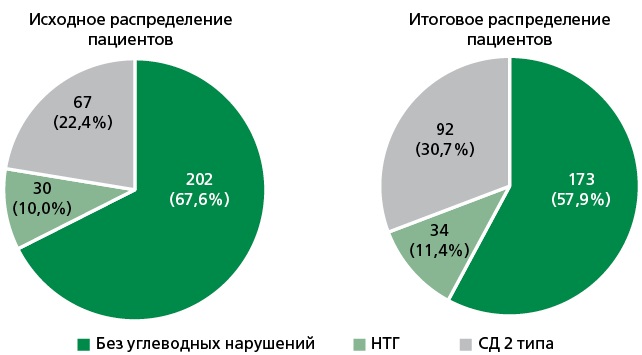
Aim. To investigate the characteristics of diagnosis and pharmacotherapy of initial carbohydrate metabolism disorders (prediabetes) in cardiology patients within the framework of an outpatient registry
Material and methods. An observational cross-sectional study was conducted as part of the outpatient registry on inappropriate prescribing practices known as CHIP (Chuvashia Inappropriate Prescribing Study). The study focused on patients over 50 years old who sought consultation from a cardiologist at the cardiology dispensary. Data from the cardiologist’s outpatient records and patients’ medical documentation were analyzed based on the registry database. The term “impaired glucose tolerance (IGT)” in the registry records was used as an equivalent to “prediabetes”. Adherence to pharmacotherapy was assessed using the adherence scale developed by the National Society of Evidence-Based Pharmacotherapy.
Results. The CHIP registry included 300 patients: 120 (40%) men and 180 (60%) women. The mean age of the participants was 66.4±7.6 years. Baseline data on the absence/presence of carbohydrate metabolism disorders in the 300 registry patients were as follows: 202 patients had no carbohydrate metabolism disorders; 30 patients were diagnosed with impaired glucose tolerance (IGT): 67 had type 2 diabetes mellitus (T2DM), and 1 had type 1 diabetes (this patient’s data were excluded from further analysis). The most common test for assessing carbohydrate metabolism was the fasting blood glucose measurement, performed in 98% of the patients; HbA1c levels were determined in 22.4% of the participants, and only 12 patients (4%) underwent an oral glucose tolerance test (OGTT). Analysis of these test results indicated that 17 patients initially classified in the “no carbohydrate disorders” subgroup had fasting blood glucose levels meeting the criteria for prediabetes, while an additional 12 individuals from this subgroup and 13 patients with an original diagnosis of IGT met the criteria for T2DM. According to final data, 173 (57.9%) individuals in the studied cohort had no carbohydrate metabolism disorders, 34 (11.4%) had prediabetes, and 92 (30.7%) had T2DM. Waist circumference and body mass index (BMI) significantly increased in the T2DM group. An increase in the frequency of comorbidities, including arterial hypertension, chronic heart failure, atrial fibrillation, and ischemic heart disease (p=0.003), as well as a history of myocardial infarction, has been observed in patients with prediabetes and diabetes mellitus compared to those without carbohydrate metabolism disorders. The highest number of patients non-adherent to pharmacotherapy was observed in the subgroup without carbohydrate disorders, while the lowest was found among patients with T2DM. Metformin was prescribed to one in five patients diagnosed with prediabetes.
Conclusion. This study highlights the incomplete diagnosis of carbohydrate metabolism disorders, specifically prediabetes and type 2 diabetes mellitus, among cardiology patients. Furthermore, it illustrates the infrequent prescription of metformin for diabetes prevention, underscoring the critical need for heightened diagnostic vigilance regarding early carbohydrate disturbances in outpatient settings, not only by endocrinologists but also by physicians from other specialties.
REVIEWS
The review reflects current data on the predictive potential of vascular stiffness (VS) indicators in relation to the risk of developing various cardiovascular (CV) events by type of CV mortality, overall mortality, the development of chronic kidney disease (CKD) and cognitive impairment, the occurrence of coronary heart disease (CHD), arterial hypertension (AH) and other outcomes. Not only pulse wave velocity (PWV), but also cardio-ankle vascular index (CAVI) is considered as indicators of VS. Its technical, physiological, clinical and other advantages are shown, especially in terms of screening. Considerable experience has been gained in using this indicator both for the clinical study of vascular status in patients with obvious CV pathology and for screening at the population level. The sources devoted to the relationship between AH and increased VS in terms of the primary and secondary nature of these shifts are analyzed. The special expediency of risk assessment using CAVI in young people in comparison with the elderly population is emphasized. Clinical and preclinical scenarios are presented in which measurement of VS using the CAVI indicator can help in risk stratification at the earliest stages of development of the vascular continuum, which corresponds to young people (YP). Current data indicate that such a need arises in the presence of isolated systolic hypertension in YP, prehypertension in people without diabetes and CKD, as well as cases of normotension with the background of an unfavorable family history of CHD. The convincing results of Russian studies of vascular screening of YP aimed at increasing the accuracy of risk assessment in them, contributing to the development of more individualized preventive intervention programs already at the early stages of CV pathology. The results of such studies will make it possible to optimize existing approaches to combating CV diseases in general by improving technologies for early primary prevention.
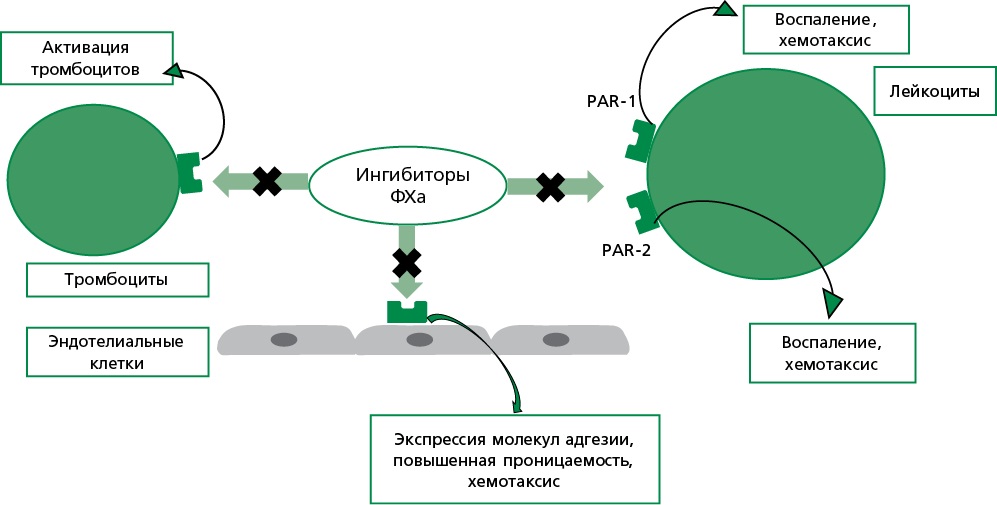
Direct oral anticoagulants (DOACs), including factor Xa inhibitors (rivaroxaban, apixaban, edoxaban) and the direct thrombin inhibitor dabigatran, are widely used for the prevention and treatment of thrombotic complications, particularly in patients undergoing major joint replacement, with atrial fibrillation (AF), as well as part of dual antithrombotic therapy (anticoagulant + antiplatelet) in patients after acute coronary syndrome and percutaneous coronary interventions, especially in the context of concomitant AF and an increased risk of systemic embolism. In recent years, there has been growing interest in studying the pleiotropic effects of DOACs that extend beyond their primary anticoagulant action on the hemostatic system. Accumulating experimental and clinical data suggest that these agents possess additional pharmacological properties — namely, anti-inflammatory, antiarrhythmic, and neuroprotective effects. The proposed molecular and cellular mechanisms include the reduction of proinflammatory cytokine levels, modulation of endothelial function, attenuation of oxidative stress, as well as favorable effects on myocardial remodeling processes and neurovascular protection. Such pleiotropic effects may play a significant pathophysiological role in slowing the progression of cardiovascular and cerebrovascular diseases, contributing to the reduction of complications and improvement of clinical outcomes. Understanding the pleiotropic properties of DOACs provides a foundation for their broader clinical application as part of integrated treatment strategies for cardiovascular, inflammatory, and cerebrovascular diseases. This review summarizes current data on the pleiotropic actions of oral anticoagulants and discusses their potential contribution to enhancing the effectiveness and individualization of pharmacotherapy in clinical cardiology.
Announcements
2025-12-29
The latest issues of 2025
Dear readers, before the New Year holidays, the latest issues are archived with long time delays. Therefore, all published issues will be posted article by article in the "Accepted for publication" section.
| More Announcements... |
ISSN 2225-3653 (Online)